Dairy consumption is associated with lower plasma dihydroceramides in women from the D.E.S.I.R. cohort
Type 2 diabetes is a multifactorial disease resulting from interactions between genetic susceptibility and environmental factors, including diet.
Sphingolipids—in particular, ceramides and dihydroceramides—have been recognized as key players in lipotoxicity, known to be associated with impaired glucose metabolism and type 2 diabetes. In the French prospective Data from the Epidemiological Study on the Insulin Resistance Syndrome (D.E.S.I.R.) cohort, it was shown that high levels of plasma ceramides and dihydroceramides are associated with type 2 diabetes, and that dihydroceramide levels are higher in people who progress to type 2 diabetes. Other recent cohort studies have yielded similar results with ceramides, but did not report on plasma dihydroceramide concentrations.
The influence of dairy product intake on type 2 diabetes risk is controversial; meta-analyses including large cohorts appear to show beneficial effects with dairy intakes. Similarly, in the D.E.S.I.R. cohort, an inverse association was shown between dairy consumption at baseline and the onset of impaired fasting glycaemia/type 2 diabetes and the metabolic syndrome over a 9-year follow-up.
Although ceramides are considered to be important cardiometabolic risk factors, there are very few published studies reporting their relationship with diet in humans and none of them concerned dairy products. Thus, the aim of the present work is to study the relationship between dairy consumption and concentrations of dihydroceramides and ceramides in the D.E.S.I.R. cohort.
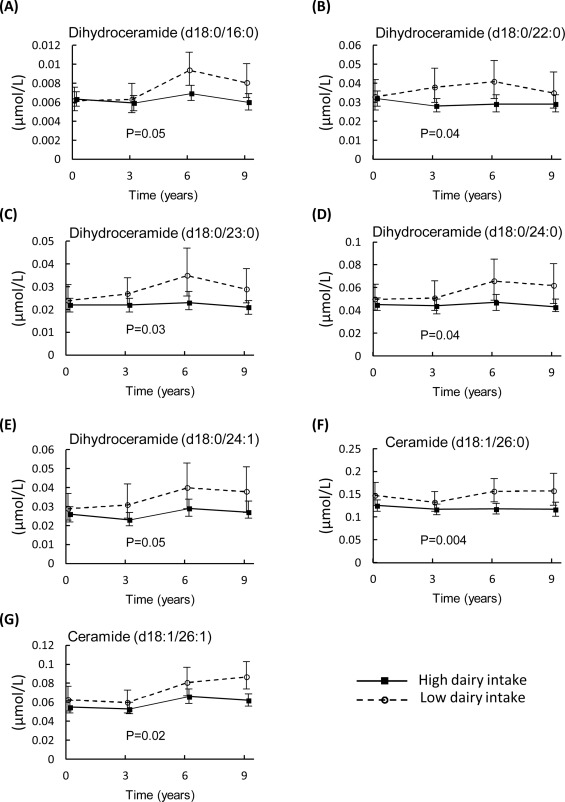
Specific plasma dihydroceramide and ceramide concentrations (A–G) in women from the Data from the Epidemiological Study on the Insulin Resistance Syndrome (D.E.S.I.R.) cohort without diabetes at either baseline or during follow-up.
To read the full paper, head to the following link:
https://www.sciencedirect.com/science/article/pii/S126236361930093X